Background: Balloon mitral valvotomy (BMV) remains an effective treatment for severe mitral stenosis secondary to rheumatic heart disease. Cardiac tamponade is a rare but life-threatening complication occurring in approximately 1-2% of cases.
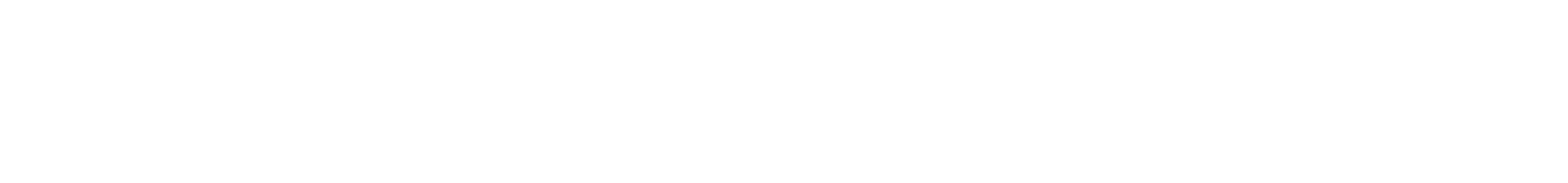
Case Presentation: We report a case of a 50-year-old female with newly diagnosed chronic rheumatic heart disease presenting with severe mitral stenosis (valve area 0.8 cm²) and a severely aneurysmal interatrial septum. During BMV, the patient developed cardiac tamponade requiring immediate pericardiocentesis. Despite this critical complication, the procedure was successfully completed with valve area increasing to 1.8 cm².
Conclusion: This case demonstrates that with prompt recognition and management of cardiac tamponade, BMV can be successfully completed even in anatomically challenging cases, offering patients significant clinical benefit while avoiding open-heart surgery.
Keywords: Balloon mitral valvotomy, cardiac tamponade, rheumatic heart disease, mitral stenosis, aneurysmal interatrial septum, pericardiocentesis
Introduction
Rheumatic heart disease (RHD) remains a significant health burden in developing countries, with mitral stenosis being the most common valvular lesion. Balloon mitral valvotomy (BMV), also known as percutaneous transvenous mitral commissurotomy (PTMC), has emerged as the preferred treatment modality for suitable candidates since its introduction in the 1980s.
While BMV is generally safe and effective, major complications can occur, including severe mitral regurgitation, systemic embolism, atrial septal defect, and cardiac perforation leading to tamponade. Studies report cardiac tamponade incidence rates between 0.5-3% during BMV procedures. The presence of anatomical variants, such as an aneurysmal interatrial septum (IAS), further increases procedural complexity and risk.
This case report illustrates the successful management of cardiac tamponade during BMV in a patient with challenging anatomy, highlighting the importance of immediate recognition, decisive intervention, and procedural expertise.
Case Presentation
Patient Information
A 50-year-old female presented to our cardiology department with progressive dyspnea on exertion for one month. The symptoms had worsened to the point where she was unable to perform routine daily activities without significant shortness of breath. She had no prior cardiac history and was newly diagnosed with chronic rheumatic heart disease.
Clinical Findings
On examination, the patient was in New York Heart Association (NYHA) functional class III-IV. Cardiovascular examination revealed:
- Regular heart rate with malar flush
- Loud first heart sound with opening snap
- Mid-diastolic murmur with presystolic accentuation at the apex
- No evidence of heart failure or peripheral edema
Diagnostic Assessment
Transthoracic Echocardiography revealed:
- Severe mitral stenosis with mitral valve area (MVA): 0.8 cm²
- Wilkins score: 9 (indicating moderate calcification and reduced leaflet mobility)
- Severely aneurysmal interatrial septum—a significant anatomical challenge for transseptal puncture
- Left atrial enlargement
- Elevated pulmonary artery pressure
- No significant mitral regurgitation
- No left atrial thrombus
ECG: Normal sinus rhythm with left atrial enlargement
Laboratory investigations: Within normal limits
Based on these findings, the patient was deemed a suitable candidate for percutaneous balloon mitral valvotomy despite the anatomical challenges posed by the aneurysmal IAS.
Therapeutic Intervention
The patient underwent BMV under fluoroscopic and echocardiographic guidance. The procedure was performed under conscious sedation with full hemodynamic monitoring.
Procedural Steps:
- Femoral venous access obtained
- Transseptal puncture attempted—complicated by severely aneurysmal IAS
- Successful transseptal catheterization achieved
- Inoue balloon positioned across the mitral valve
- Sequential balloon inflations performed
Critical Complication:
During the procedure, the patient developed acute hemodynamic instability with:
- Sudden drop in blood pressure
- Elevated jugular venous pressure
- Muffled heart sounds
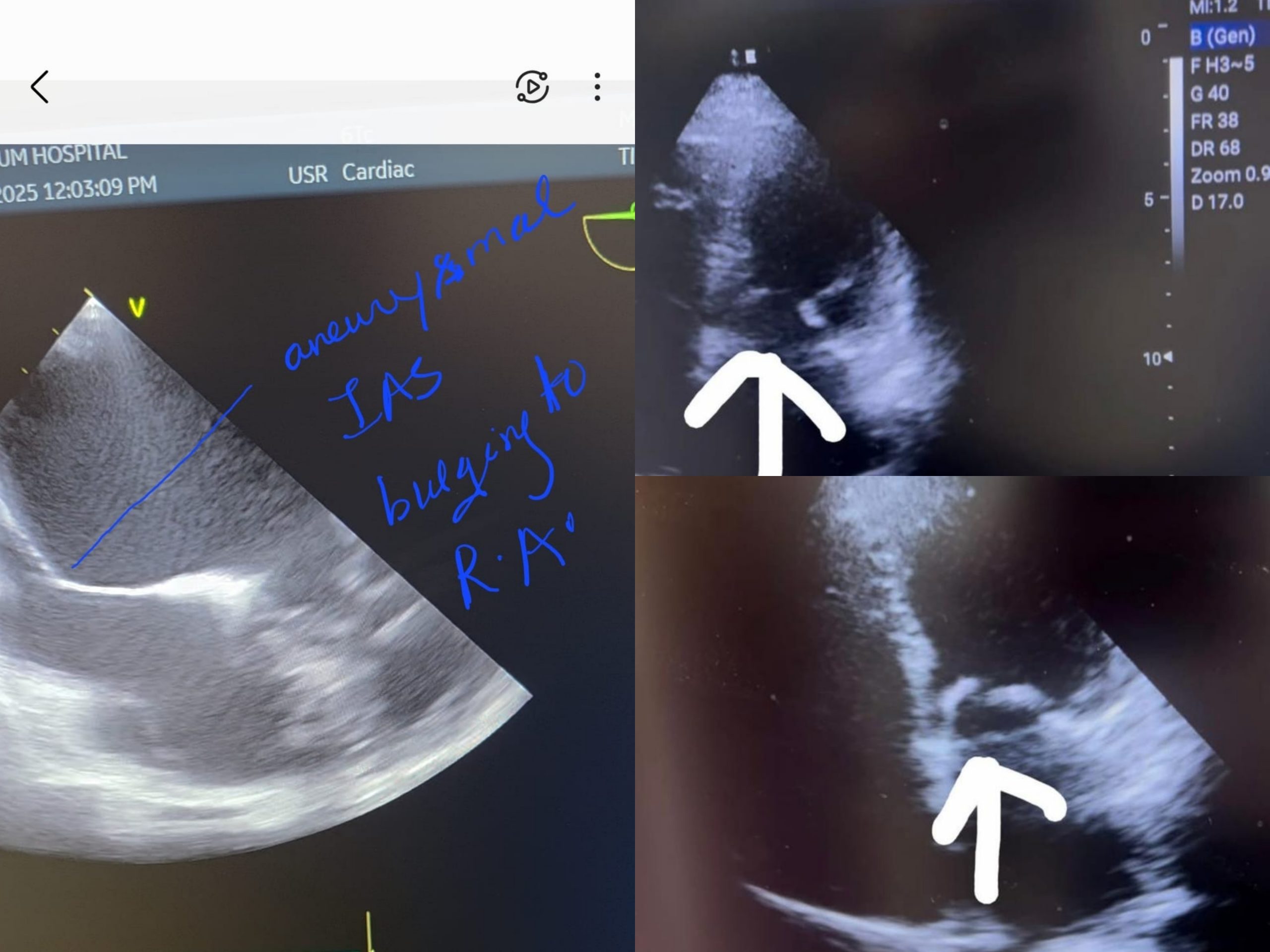
Immediate bedside echocardiography confirmed cardiac tamponade with:
- Moderate to large pericardial effusion
- Right atrial and ventricular diastolic collapse
- Hemodynamic compromise
Emergency Management:
- Procedure temporarily halted
- Immediate pericardiocentesis performed under echocardiographic guidance
- Approximately 200-250 ml of hemorrhagic fluid was aspirated
- Hemodynamic stability restored
- Pericardial drain left in situ
Decision Point:
Following stabilization and multidisciplinary team discussion, the decision was made to continue the BMV procedure rather than abort and refer for emergency cardiac surgery. This decision was based on:
- Successful hemodynamic stabilization
- Controlled drainage via pericardial catheter
- Patient’s informed consent
- Availability of cardiac surgical backup
Completion of Procedure:
The BMV was successfully completed with:
- Final mitral valve area: 1.8 cm² (125% increase from baseline)
- Significant reduction in transmitral gradient
- No significant mitral regurgitation
- Stable hemodynamics were maintained throughout completion
Outcome and Follow-up
Immediate Post-Procedure:
- Patient transferred to cardiac ICU for close monitoring
- Pericardial drain output monitored (minimal drainage after initial event)
- Serial echocardiograms showed no reaccumulation of pericardial fluid
- Hemodynamically stable throughout ICU stay
Hospital Course:
- Drain removed on post-procedure day 2
- Gradual improvement in functional capacity
- No complications during hospitalization
- Discharged on post-procedure day 5 in stable condition
Follow-up (Outpatient):
- Symptomatic improvement to NYHA Class I
- Able to perform daily activities without dyspnea
- Follow-up echocardiography confirmed:
- Maintained valve area of 1.8 cm²
- No mitral regurgitation
- No residual pericardial effusion
- Improved left atrial pressures
The patient avoided:
- Sternotomy
- Cardiopulmonary bypass
- Mitral valve replacement surgery
- Extended hospital stay
- Prolonged recovery period
Discussion
Significance of the Case
This case highlights several important aspects of interventional cardiology practice:
- Anatomical Challenges:
The presence of a severely aneurysmal interatrial septum poses significant technical difficulty during transseptal puncture. The distorted anatomy increases the risk of cardiac perforation, which likely contributed to the tamponade in this case. Studies show that anatomical variants increase procedural complexity and complication rates. - Cardiac Tamponade During BMV:
Literature reports cardiac tamponade incidence of 0.5-3% during BMV procedures. Mechanisms include:
- Perforation during transseptal puncture
- Left atrial appendage perforation
- Ventricular perforation by guidewire or balloon
- “Stitch phenomenon” (needle piercing from the right atrium through the pericardium back into the left atrium)
Joseph et al. described mechanisms of cardiac perforation in 10 cases among 903 BMV procedures (1.1%), emphasizing the importance of recognizing perforation sites and immediate management.
- Crisis Management:
Immediate recognition of cardiac tamponade through clinical signs and bedside echocardiography was crucial. The classic Beck’s triad (hypotension, elevated jugular venous pressure, muffled heart sounds) combined with echo findings allowed rapid diagnosis.
Pericardiocentesis restored hemodynamic stability, but the critical decision was whether to:
- Abort the procedure and refer for surgery (leaving the patient with unsuccessful BMV and requiring emergency MVR)
- Continue after stabilization (completing the intended therapeutic intervention)
- Risk-Benefit Analysis:
The decision to continue was based on:
- Patient benefit: Completing BMV would provide immediate therapeutic benefit, potentially adding 8-10 years before surgical intervention is needed
- Technical feasibility: Hemodynamic stability achieved, drainage controlled
- Surgical backup: Immediate availability if needed
- Operator expertise: Team is experienced in managing complex cases
- Long-term Implications:
A successful BMV increasing valve area from 0.8 to 1.8 cm² offers:
- Immediate symptom relief
- Improved quality of life
- Delay in the need for valve replacement surgery by approximately 8-10 years
- Avoidance of cardiopulmonary bypass complications
- Shorter hospital stay and recovery
- Cost-effectiveness compared to surgical intervention
Clinical Lessons
For Interventional Cardiologists:
- Thorough pre-procedural imaging to identify anatomical challenges
- Heightened vigilance during transseptal puncture in patients with IAS abnormalities
- Immediate availability of echocardiography during procedure
- Preparedness for rapid pericardiocentesis
- Multidisciplinary team approach for crisis decision-making
BMV as a “Dying Art”:
As noted in this case, BMV is becoming less commonly performed despite its effectiveness. This trend is concerning because:
- BMV offers excellent outcomes in appropriate candidates
- It’s less invasive than surgery
- Cost-effective for resource-limited settings
- Requires specialized training and experience
- Training opportunities are decreasing as volumes decline
The mentor’s quote—”BMV is a service to mankind, offering maximum benefit to the patient, minimal benefit to the doctor, and maximum headache throughout”—captures the essence of this procedure: technically demanding, financially less rewarding than surgery, but profoundly beneficial for patients.
Comparison with Literature
Studies on very late follow-up of BMV show:
- Procedural success rates of 85-90%
- Restenosis-free survival: 85% at 5 years, 60% at 10 years
- Predictors of restenosis include left atrial size and pre/post-procedural gradients
- Even with restenosis, repeat BMV can be performed successfully
This case aligns with published outcomes, demonstrating that despite major complications, expert management can achieve excellent results.
Conclusion
This case demonstrates that cardiac tamponade during BMV, while life-threatening, can be successfully managed with prompt recognition, immediate intervention, and expert decision-making. The successful completion of BMV despite this major complication resulted in significant clinical benefit for the patient, who avoided open-heart surgery and achieved substantial symptom improvement.
Key takeaways include:
- Anatomical variants like aneurysmal IAS increase procedural complexity
- Immediate echocardiographic assessment is crucial for diagnosing tamponade
- Pericardiocentesis can stabilize patients and allow procedure completion
- Risk-benefit analysis must be individualized
- BMV remains a valuable therapeutic option that can provide years of benefit
This case reinforces the importance of maintaining BMV expertise within the cardiology community and highlights the rewards of this “service to mankind” when performed by experienced operators with appropriate support systems in place.
Learning Points
- Severe mitral stenosis with challenging anatomy can be successfully treated with BMV
- Cardiac tamponade during BMV requires immediate recognition and pericardiocentesis
- Continuing a procedure after stabilizing a major complication may be appropriate in select cases
- BMV can delay the need for surgical valve replacement by approximately a decade
- Multidisciplinary teamwork is essential for managing procedural complications
- BMV expertise should be preserved and transmitted to future cardiologists
Patient Perspective
The patient expressed profound gratitude for avoiding open-heart surgery and reported significant improvement in quality of life, being able to return to normal daily activities without breathlessness within weeks of the procedure.
Acknowledgments
This case was managed through the collaborative efforts of the entire catheterization laboratory team. Special acknowledgment to:
- Dr. P.K. Dash – Mentor and guide whose teaching and expertise were instrumental
- Deepak (supporting physician) – Critical support during the crisis
- Tapas (cath lab technician) – Technical expertise
- Resident team – Vigilance and composure during the emergency
- Nursing staff – Excellent post-procedural care
Author Information
Dr. Gyana Ranjan Nayak
Interventional Cardiologist
Bhubaneswar, Odisha, India
Specialization: Complex coronary interventions, structural heart disease, balloon mitral valvotomy
References
- Joseph G, et al. Mechanisms of cardiac perforation leading to tamponade during balloon mitral valvuloplasty. Catheter Cardiovasc Diagn. 1997;42(2):138-146.
- Pan M, et al. Cardiac tamponade complicating mitral balloon valvuloplasty. Am J Med. 1991.
- Seca L, Costa M, et al. Percutaneous Mitral Valvuloplasty Complicated by Cardiac Tamponade in a Pregnant Patient. Arq Bras Cardiol. 2008;91(5):e53-e55.
- Very Late Follow-up of Percutaneous Balloon Mitral Valvotomy. Rev Bras Cardiol Invasiva. 2012.
- Cleveland Clinic. Cardiac Tamponade: Symptoms & Causes. 2025.
- StatPearls. Cardiac Tamponade. NCBI Bookshelf. 2023.
Correspondence:
Dr. Gyana Ranjan Nayak
Phone: 6371307504