Background
Critical limb ischemia in patients under 65 presents unique diagnostic and therapeutic challenges, particularly when caused by infrarenal aortic stenosis. Conventional femoral access becomes impossible when bilateral femoral pulses are absent.
Case Presentation: We report a case of a 62-year-old male presenting with severe claudication, critical limb ischemia, and arterial ulcers. Angiography revealed critical infrarenal aortic stenosis with absent bilateral femoral pulses, eliminating standard access routes. Using a hybrid radial-to-femoral approach, initial angioplasty was performed via radial access, restoring femoral pulses and allowing completion via femoral access with stent deployment.
Conclusion: This case demonstrates that innovative access strategies can mean the difference between amputation and limb salvage. When traditional approaches are unavailable, adaptive procedural planning enables successful revascularization even in technically challenging scenarios.
Keywords: Critical limb ischemia, infrarenal aortic stenosis, radial access, limb salvage, peripheral arterial disease, hybrid endovascular technique
Introduction
Peripheral arterial disease (PAD) with critical limb ischemia represents a limb-threatening condition requiring urgent intervention. In younger patients (under 65 years), the disease progression is typically more aggressive, with studies showing a 24% higher amputation risk compared to older populations. This aggressive trajectory makes timely revascularization critical for limb salvage and functional recovery.
Endovascular interventions for aortoiliac occlusive disease traditionally rely on femoral artery access. However, when severe infrarenal aortic stenosis completely obliterates distal flow, standard access routes become impossible. In these scenarios, alternative approaches are necessary to achieve successful revascularization.
This case report illustrates a hybrid radial-to-femoral technique for managing critical infrarenal aortic stenosis when conventional femoral access was unavailable, highlighting the importance of procedural versatility in complex vascular interventions.
Case Presentation
Patient Information
A 62-year-old male presented to our cardiology department with progressive symptoms of severe claudication and critical limb ischemia. The patient reported inability to walk more than a few meters without significant pain and had developed non-healing arterial ulcers on both lower extremities.
Clinical Findings
On examination, the patient demonstrated:
- Severe bilateral lower extremity claudication
- Arterial ulcers consistent with critical limb ischemia
- Absent bilateral femoral pulses—a critical finding indicating severe proximal obstruction
- Cool lower extremities with poor capillary refill
- No palpable pedal pulses bilaterally
The absence of femoral pulses raised immediate concern about procedural access for potential endovascular intervention.
Diagnostic Assessment
Angiography revealed:
- Critical stenosis of the infrarenal aorta with near-complete occlusion
- Severely reduced distal arterial flow
- Patent distal vessels suitable for revascularization if proximal flow could be restored
- No alternative collateral pathways providing adequate perfusion

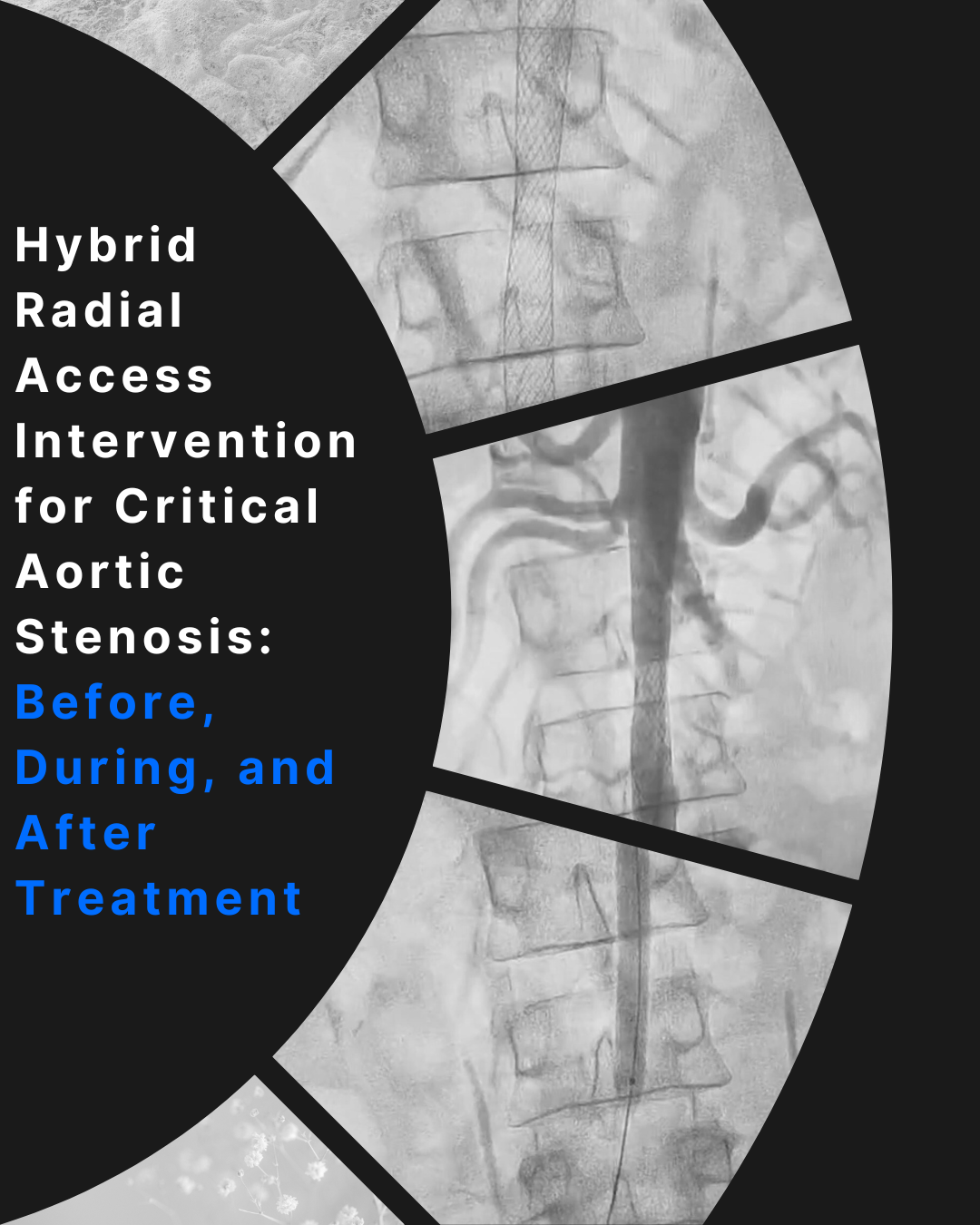
Figure 1: Pre-intervention angiography demonstrating critical infrarenal aortic stenosis with severe flow limitation and absent bilateral femoral pulses
Clinical Risk Stratification:
Given the patient’s age (under 65) and aggressive disease presentation, the 24% elevated amputation risk made immediate intervention imperative. Without successful revascularization, bilateral amputation was highly probable within months.
Therapeutic Intervention
The patient underwent endovascular intervention with a novel hybrid approach necessitated by anatomical constraints.
Procedural Challenge:
Standard femoral access—the conventional approach for aortic interventions—was impossible due to absent femoral pulses. The critical stenosis had completely eliminated distal arterial flow, making femoral puncture unfeasible.
Innovative Solution: Hybrid Radial-to-Femoral Approach
Phase 1: Radial Access Angioplasty
- Right radial (wrist) artery access obtained
- Diagnostic catheter advanced retrograde through the brachial and subclavian arteries into the thoracic aorta
- Catheter navigated down the descending aorta to the site of infrarenal stenosis
- Guidewire carefully advanced across the critical stenosis
- Balloon angioplasty catheter positioned at the stenotic segment
- Sequential balloon inflations performed to dilate the infrarenal aorta
Critical Moment:
Upon successful dilation of the stenosis, bilateral femoral pulses immediately returned—a dramatic and clinically significant finding indicating restoration of distal arterial flow.
Phase 2: Femoral Access Completion
With femoral pulses now palpable:
- Right femoral artery access obtained
- Upsized access achieved for larger device delivery
- Self-expanding wallstent deployed across the infrarenal aortic stenosis
- Final angiography confirmed excellent stent deployment with restored flow
- Both femoral pulses remained strong and palpable

Figure 2: Intra-procedural image showing self-expanding wallstent deployment across the infrarenal aortic stenosis following successful radial access angioplasty
Outcome and Follow-up
Immediate Post-Procedure:
The results were remarkable:
- Patient ambulating independently in the hospital corridor within 24 hours
- Complete resolution of rest pain
- Strong bilateral femoral and pedal pulses
- Improved lower extremity perfusion with warmer skin temperature

Figure 3: Post-intervention angiography demonstrating excellent stent expansion with complete restoration of arterial flow and palpable bilateral femoral pulses
Hospital Course:
- No procedural complications
- Progressive improvement in mobility
- Arterial ulcers beginning to show signs of healing
- Discharged on post-procedure day 3 in stable condition
Follow-up (Outpatient):
At subsequent follow-up visits:
- Patient walking 2 to 3 kilometers daily without symptoms
- Complete healing of arterial ulcers
- Maintained strong bilateral pulses
- No claudication symptoms
- Full functional recovery with excellent quality of life
The patient avoided:
- Bilateral amputation
- Open surgical aortic reconstruction
- Prolonged hospitalization
- Permanent disability
Discussion
Significance of the Case
This case highlights several critical aspects of complex vascular interventions:
Anatomical Challenges:
Critical infrarenal aortic stenosis with absent femoral pulses presents a unique technical challenge. Standard femoral access—the workhorse approach for aortoiliac interventions—becomes impossible when the very pathology requiring treatment prevents access to the treatment site.
Age-Specific Risk in Critical Limb Ischemia:
Younger patients with PAD face distinct challenges:
- More aggressive disease progression
- 24% higher amputation risk compared to older populations
- Greater functional impact due to active lifestyle requirements
- Longer life expectancy making limb salvage even more crucial
The Hybrid Radial-to-Femoral Technique:
This case demonstrates procedural innovation when faced with anatomical constraints:
Step 1 (Radial Approach): Using transradial access allowed navigation from the upper extremity arterial system down to the infrarenal aorta, bypassing the need for femoral pulses entirely.
Step 2 (Flow Restoration): Initial balloon angioplasty restored sufficient flow to generate palpable femoral pulses—essentially creating the access route needed for definitive treatment.
Step 3 (Femoral Completion): With femoral access now possible, larger devices could be delivered for optimal stent deployment.
Crisis Management and Adaptive Planning:
“This case demonstrates how adaptive procedural planning can mean the difference between amputation and full recovery,” said Dr. Gyana Ranjan Nayak. “When traditional access routes are unavailable, interventional cardiologists must have alternative strategies ready to save both limbs and lives.”
The decision to pursue this hybrid approach was based on:
- Clinical urgency: High amputation risk without intervention
- Technical feasibility: Radial access capable of reaching target lesion
- Anatomical suitability: Viable distal vessels if proximal flow restored
- Operator expertise: Experience with complex access techniques
Clinical Lessons
For Interventional Cardiologists:
- Radial access can serve as alternative route when femoral access is unavailable
- Sequential procedural strategy (radial first, then femoral) enables successful treatment in challenging anatomy
- Immediate return of femoral pulses after proximal angioplasty confirms successful revascularization
- Younger patients with critical limb ischemia require aggressive intervention given elevated amputation risk
- Technical versatility and willingness to adapt standard approaches are essential for complex vascular cases
Conclusion
This case demonstrates that when confronted with technical challenges that eliminate standard access routes, innovative procedural strategies can achieve successful revascularization and limb salvage. The hybrid radial-to-femoral approach enabled treatment of critical infrarenal aortic stenosis despite absent femoral pulses, resulting in dramatic clinical improvement and avoiding bilateral amputation.
Key Takeaways:
- Radial access serves as effective alternative when femoral access is impossible
- Initial balloon angioplasty can restore flow sufficiently to enable secondary access
- Younger patients with critical limb ischemia warrant aggressive intervention given elevated amputation risk
- Procedural versatility and adaptive planning are essential for complex vascular cases
- Successful revascularization provides life-changing functional recovery
This case reinforces the importance of technical innovation in interventional cardiology and the life-changing impact of timely, creative approaches to limb-threatening ischemia.
Learning Points
- Critical limb ischemia in patients under 65 carries 24% higher amputation risk
- Absent femoral pulses indicate severe proximal disease but don’t preclude intervention
- Radial access can reach infrarenal aortic lesions when femoral access unavailable
- Restoring flow via balloon angioplasty may create new access options mid-procedure
- Hybrid access strategies enable successful treatment in anatomically challenging cases
- Early intervention in younger patients provides decades of functional benefit
Patient Perspective
The patient expressed profound relief at avoiding amputation and reported that regaining the ability to walk normally “gave me my life back.” He has returned to all normal activities and remains symptom-free at follow-up.
About Dr. Gyana Ranjan Nayak
Dr. Gyana Ranjan Nayak is an interventional cardiologist in Bhubaneswar specializing in complex vascular and structural heart procedures. His practice focuses on limb-salvage interventions, critical aortic disease management, and advanced cardiovascular care.
Specializations:
- Complex peripheral arterial disease interventions
- Limb salvage procedures
- Aortoiliac revascularization
- Structural heart interventions
Correspondence:
Dr. Gyana Ranjan Nayak
Phone: 6371307504
Website: drgyana.com
References
- Norgren L, Hiatt WR, Dormandy JA, et al. Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II). J Vasc Surg. 2007;45 Suppl S:S5-67.
- Conte MS, Bradbury AW, Kolh P, et al. Global vascular guidelines on the management of chronic limb-threatening ischemia. J Vasc Surg. 2019;69(6S):3S-125S.
- Gerhard-Herman MD, Gornik HL, Barrett C, et al. 2016 AHA/ACC Guideline on the Management of Patients With Lower Extremity Peripheral Artery Disease. Circulation. 2017;135(12):e726-e779.
- Aboyans V, Ricco JB, Bartelink ML, et al. 2017 ESC Guidelines on the Diagnosis and Treatment of Peripheral Arterial Diseases. Eur Heart J. 2018;39(9):763-816.
- Mills JL Sr, Conte MS, Armstrong DG, et al. The Society for Vascular Surgery Lower Extremity Threatened Limb Classification System. J Vasc Surg. 2014;59(1):220-234.
- Almasri J, Adusumalli J, Asi N, et al. A systematic review and meta-analysis of revascularization outcomes of infrainguinal chronic limb-threatening ischemia. J Vasc Surg. 2018;68(2):624-633.
- Jolly SS, Yusuf S, Cairns J, et al. Radial versus femoral access for coronary angiography and intervention in patients with acute coronary syndromes (RIVAL): a randomised, parallel group, multicentre trial. Lancet. 2011;377(9775):1409-1420.
- Kovacic JC, Sharma AB, Roy S, et al. Radial Access Approach to Peripheral Vascular Interventions. Circ Cardiovasc Interv. 2024;17(1):e013606.
- Dotter CT, Judkins MP. Transluminal treatment of arteriosclerotic obstruction. Circulation. 1964;30:654-670.
- Bosiers M, Deloose K, Verbist J, Peeters P. Self-expanding stents and aortoiliac occlusive disease. J Cardiovasc Surg (Torino). 2014;55(2 Suppl 1):25-32.
- Jongkind V, Akkersdijk GJ, Yeung KK, Wisselink W. A systematic review of endovascular treatment of extensive aortoiliac occlusive disease. J Vasc Surg. 2010;52(5):1376-1383.
- Indes JE, Pfaff MJ, Farrokhyar F, et al. Clinical outcomes of 5358 patients undergoing direct open bypass or endovascular treatment for aortoiliac occlusive disease: a systematic review and meta-analysis. J Endovasc Ther. 2013;20(4):443-455.