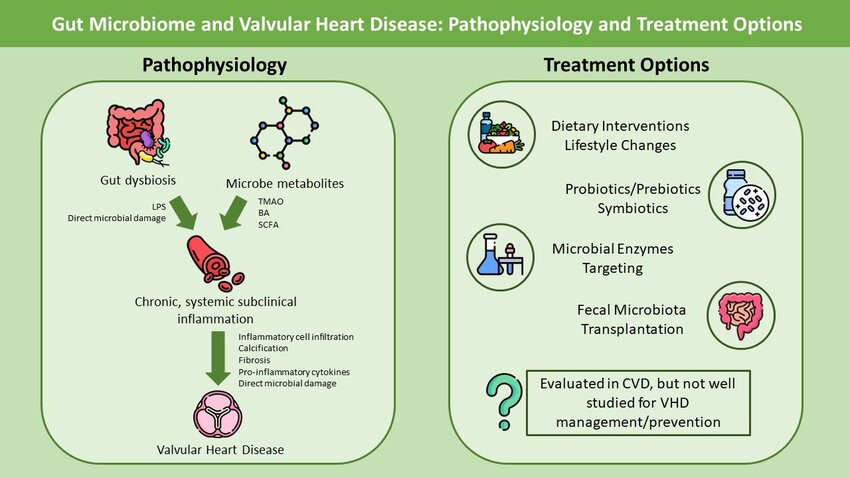
Recent research has shed light on the significant connection between the gut microbiome (GM) and cardiovascular disease (CVD). While it’s well-established that gut dysbiosis plays a role in conditions like hypertension, dyslipidemia, and heart failure, its involvement in valvular heart disease (VHD) is less understood. However, emerging data suggests that the gut microbiome may play a critical role in the development and progression of VHD through systemic inflammation and metabolic pathways.
Case Overview
A 65-year-old male patient with a history of mild mitral valve regurgitation presented with worsening symptoms, including fatigue and shortness of breath. Over the past two years, the patient had also experienced gastrointestinal issues such as bloating and irregular bowel movements, which had been dismissed as unrelated to his cardiac condition. However, recent studies have revealed a potential link between gut dysbiosis and valvular heart dysfunction, prompting a more thorough investigation into his gut health.
Diagnostic Approach
The patient underwent comprehensive testing, which included an analysis of his gut microbiome through stool sample testing, along with echocardiography to assess the progression of his mitral valve disease. The gut microbiome analysis revealed significant dysbiosis, with an overgrowth of inflammatory-promoting bacteria and a reduction in beneficial microbial diversity. The echocardiogram showed moderate progression of mitral valve calcification and fibrosis.
Pathophysiology Link
The connection between gut dysbiosis and valvular disease is now better understood. Dysbiosis leads to chronic low-grade systemic inflammation, which promotes the infiltration of inflammatory cells into heart valves. This inflammatory response, mediated by pro-inflammatory molecules, triggers a cascade of events that result in valve calcification, fibrosis, and eventual dysfunction. Environmental factors, including diet and lifestyle, further exacerbate this gut-heart axis.
Therapeutic Intervention
Based on the growing body of evidence, a multidisciplinary treatment plan was implemented, focusing on restoring gut microbiome balance to reduce inflammation and slow the progression of valvular disease. The patient’s regimen included:
- Dietary Modifications: A gut-friendly diet rich in fiber, prebiotics, and anti-inflammatory foods was prescribed. This included more fruits, vegetables, whole grains, and fermented foods.
- Probiotics and Prebiotics: A combination of probiotic supplements and prebiotic fibers was introduced to restore microbial balance and promote the growth of beneficial bacteria.
- Lifestyle Changes: The patient was encouraged to adopt regular physical activity, stress management techniques, and better sleep hygiene to positively influence his gut health.
- Fecal Microbiota Transplant (FMT): After initial improvement, the patient underwent FMT, a treatment still considered experimental but showing promising results in altering gut microbiome composition and reducing systemic inflammation.
Outcome
Over the course of six months, the patient reported significant improvements in his gastrointestinal symptoms, overall energy levels, and breathing. Follow-up testing showed a marked reduction in systemic inflammation and stabilization of his valvular heart disease progression. While mitral valve dysfunction remained present, the rate of deterioration had slowed, and the patient experienced an improved quality of life.
Conclusion
This case highlights the emerging link between the gut microbiome and valvular heart disease, offering new therapeutic avenues for patients with VHD. By addressing gut health through dietary changes, probiotics, and potentially FMT, it is possible to influence the inflammatory state that contributes to valve calcification and fibrosis. More research is needed, but current evidence suggests that gut-targeted therapies may hold significant potential in managing and preventing valvular heart disease progression.
This case underscores the importance of a holistic approach to heart health, recognizing the gut-heart connection and the need for personalized treatment plans that address both cardiac and microbiome health.